Background
Before the COVID-19 pandemic, the WHO described vaccine hesitancy as one of the ‘ten greatest challenges to global health’[1]. Vaccination represents the best chance to escape the current public health restrictions. Apart from the logistical challenges of vaccine development, procurement, delivery, storage and injection, it will also be necessary to manage vaccine hesitancy within the community.
Vaccination is one of the most cost-effective ways of avoiding disease – it currently prevents 2 - 3 million deaths a year, and a further 1.5 million could be avoided if global coverage of vaccinations improved[2].
A study recently published in Hong Kong suggested low levels of vaccine acceptance for COVID-19[3]. The overall vaccine acceptance rate after adjustment for population distribution was 37.2%. This study was undertaken in July and August 2020 at the height of the third wave. Other international studies taken around the same time showed higher levels of acceptance. A large international review published in Nature in October 2020 suggested that 71.5% of people worldwide would be very or somewhat likely to take a COVID-19 vaccine[4]. An ongoing Hong Kong University survey showed that 46% of respondents intended to get vaccinated in January 2021 whereas back in November 2020 63% had indicated that they would accept vaccination. This is compatible with a number of international studies which show intention varying over time but relatively high rates of vaccine hesitancy in Hong Kong.
We undertook an email survey in order to identify current perceptions of COVID-19 vaccination within our population. Our goal was to identify current intentions in addition to vaccine preference. We were also looking to identify potential barriers to immunisation within our patient population.
Method
The survey comprised an e-questionnaire. The questionnaire was included in a regular COVID-19 update which is emailed to all OT&P patients who have requested inclusion in the newsletter database in addition to all OT&P staff. The newsletter included a link to an article on COVID-19 vaccination and a podcast in which vaccination was discussed.
Result
We received 1,020 responses. The demographic data is summarised below. This cohort tends to be older and more international than a typical Hong Kong population.
| Total numbers by age including patients + doctors + staff |
|
| Age Group | Grand Total |
| ≥ 60 | 196 |
| 35 - 59 | 681 |
| 19 - 34 | 143 |
| Grand Total | 1020 |
Only 14% are under 35 years of age and 77% are permanent Hong Kong residents.
| Do you intend to be vaccinated? Patients + doctors + staff |
|
| Yes | 877 (86%) |
| No | 143 (14%) |
| Grand Total | 1020 (100%) |
Of the total number who responded, 86% indicated that they intended to be vaccinated and 14% indicated that they would not.
| Do you intend to be vaccinated? Patient only excluding OT&P Staff |
|
| Yes | 810 (90.4%) |
| No | 86 (9.6%) |
| Grand Total | 896 (100%) |
Excluding OT&P staff, 90.4% (810/896) of patients indicated that they would be vaccinated whereas 9.6% (86/896) indicated that they would not.
| Do you intend to be vaccinated? Female v Male |
||
| Gender | Female (n = 496) | Male (n = 427) |
| Yes | 418 | 392 |
| No | 51 | 35 |
| Percentage to Yes | 84.27% | 91.80% |
The patient cohort showed a gender difference with males 91.80% (392/427) being more likely to answer yes to vaccination than females 84.27% (418/469).
| Do you intend to be vaccinated? Doctor and non-medical staff |
||||
| Occupation | Yes | No | Grand Total | % Yes |
| Doctor | 22 | 3 | 25 | 88% |
| Staff excluding doctors | 45 | 54 | 99 | 45% |
Within the respondents from OT&P staff, 88% (22/25) of doctors intend to be vaccinated in comparison to 45% staff excluding doctors.
| Do you intend to be vaccinated? Patient: Age < 35 and Age > 35 |
||||
| Age | Yes | No | Grand Total | % Yes |
| < 35 | 83 | 15 | 98 | 85% |
| > 35 | 727 | 71 | 798 | 91% |
In the patient cohort there was a small difference in intention to vaccinate for those under 35 years of age 85% (83/98) in comparison to those older than 35 years of age 91% (727/798).
| Do you intend to be vaccinated? Other Staffs: Age < 35 and Age > 35 |
||||
| Age | Yes | No | Grand Total | % Yes |
| < 35 | 14 | 30 | 44 | 32% |
| > 35 | 31 | 24 | 55 | 56% |
This was more marked in OT&P staff. In staff aged 34 years and younger, 32% (14/44) responded yes to vaccination. Those 35 and older 56% (31/55) indicated yes. Of staff over 60 years 100% (3/3) indicated yes.
| Preference on vaccine |
||
| Vaccine | Grand Total | Percentage |
| No preference/First available vaccine | 137 | 16% |
| Oxford-AstraZeneca | 257 | 29% |
| Pfizer-BioNTech | 453 | 52% |
| Sinovac-Biotech | 30 | 3% |
| Grand Total | 877 | 100% |
When asked for current vaccine preference, 16% (137/877) expressed no preference/a preference for the first available vaccine. 52% (453/877) preferred Pfizer-BioNtech, 29% (257/877) Oxford-AstraZeneca and 3% (30/877) Sinovac-Biotech.
Only respondents who indicated that they would not take the vaccination were asked the following questions:
| Additional questions | ||
| Yes | No | |
| Would be more likely to take the vaccine if they received financial payment | 4% | 96% |
| Would be more likely to take the vaccine if a vaccine certificate was required for international travel | 65% | 35% |
Discussion
There are clear limitations to this survey. It was an email survey conducted in English with recognised and acknowledged potential for selection bias. It is an assessment of intention to vaccinate rather than a retrospective review. The OT&P demographic is not truly representative of the Hong Kong population. This cohort is older, more international and is skewed in terms of educational and socioeconomic factors. It is a snapshot in time of a particular population.
This cohort of patients have engaged with ongoing public health content via OT&P newsletters and generally have a positive view towards vaccination for COVID-19. The intended uptake is high in comparison to other studies. 90.4% of OT&P patients who responded to this survey indicate an intention to vaccinate. How representative this cohort is of final numbers in Hong Kong will be interesting to compare.
The population of patients who completed this survey have the same intention to vaccinate 90.4% (810/896) as OT&P doctors 88% (22/25) and significantly higher than non-doctor OT&P staff 45% (45/99). The uptake in OT&P staff (45%) is very similar to the Hong Kong University population sample (46%) taken over the same time.
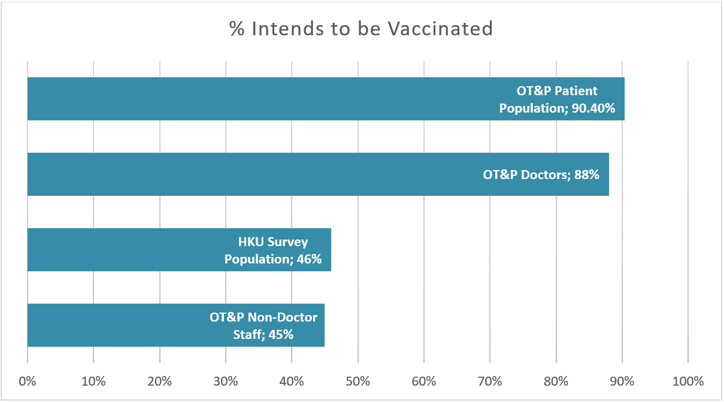
Fig 1. A graph showing the percentage of people that intends to be vaccinated across different populations from our survey and the University of Hong Kong's recent survey.
In this patient cohort males (92%) are more likely to answer yes to vaccination than females (84%). Previous studies have suggested that younger participants are less likely to vaccinate. Patients under 35 in the patient survey indicated relatively high intention to vaccinate (85%) compared to only 32% in the OT&P staff survey.
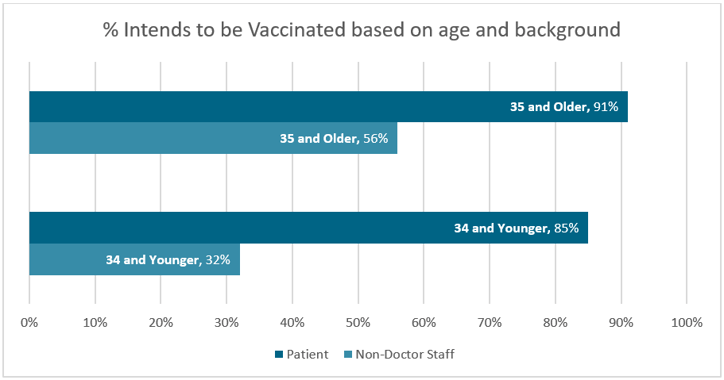
Fig 2. The difference in the intension to be vaccinated among OT&P non-doctor staff and OT&P general population
The HKU survey suggested higher vaccine hesitancy with younger age which is compatible with the OT&P staff cohort but the OT&P younger patients are significantly more likely to express intention to vaccinate. The HKU survey also suggested increasing vaccine hesitancy with higher educational and income levels. This would appear to be a direct contradiction with our findings of very high vaccine acceptance in a population with a higher socioeconomic and educational bias. This is certainly an avenue for further research.
There is a clear, relative preference for either the Pfizer-BioNtech or Oxford-AstraZeneca vaccines. Although 16% (137/877) of the total cohort expressed no preference, of those who did express a preference only 4% (30/740) indicated Sinovac-Biotech as first choice. It seems logical that this relates to the lower reported effectiveness and the mixed messaging associated with release of clinical trials data. We have described in a previous article the different measures of vaccine effectiveness. Managing this messaging within Hong Kong will be a key challenge in increasing vaccine uptake.
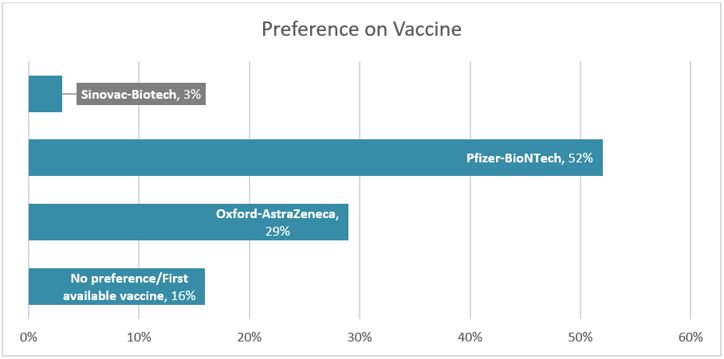
Fig 3. Preferences on vaccine based on OT&P surveyed population
The reasons for not vaccinating both in specific answers and in free text were in the majority related to issues of vaccine safety. 83% of respondents who declined vaccination cited vaccine safety, 10% because the vaccine was rushed (a surrogate for safety concerns) and 3% expressed scepticism of the severity of COVID-19 as disease.
Philosophical arguments on increasing vaccine uptake tend to range from encourage at one end of the spectrum to mandate at the other. In between there are a range of interventions, many of which can be adopted from theories of behavioural economics. This may range from ‘nudges’ which are not explicitly economic or value based to those which explicitly give a reward/penalty. At least within our population, individuals who indicate vaccine hesitancy are significantly more likely to be encouraged by the possibility of easier and/or quarantine free travel 65% than they are by a financial incentive 4%. In other population groups this may well be reversed.
Ultimately, education and honest information are key factors in managing epidemics. We have consistently expressed the opinion that Hong Kong has world class systems and expertise in the management of infectious disease. There is a strong tradition of Public Health, Virology and Epidemiology which is recognised internationally. Public health interventions must balance our increasing and evolving understanding of the impact of the disease on both individuals and the health system with the social and economic costs of the interventions within the specific context of the social, cultural and economic needs of the people of Hong Kong. High uptake of an effective vaccine represents the best opportunity for Hong Kong to normalise the current public health restrictions. This will require consistent honest but positive messaging around the evidence of the benefits of vaccination in addition to creative strategies for managing vaccine hesitancy in demographics with higher vaccine scepticism and lower uptake.
Reference
1. “Ten Health Issues WHO Will Tackle This Year.” World Health Organization, World Health Organization, www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
2. “Immunization.” World Health Organization, World Health Organization, www.who.int/news-room/facts-in-pictures/detail/immunization.
3. Wong, Martin C.S., et al. “Acceptance of the COVID-19 Vaccine Based on the Health Belief Model: A Population-Based Survey in Hong Kong.” Vaccine, Elsevier, 6 Jan. 2021, www.sciencedirect.com/science/article/pii/S0264410X20316959.
4. Lazarus, Jeffrey V., et al. “A Global Survey of Potential Acceptance of a COVID-19 Vaccine.” Nature News, Nature Publishing Group, 20 Oct. 2020, www.nature.com/articles/s41591-020-1124-9.
 Central General Practice
Central General Practice
 Repulse Bay
Repulse Bay
 Clearwater Bay
Clearwater Bay
 Central Specialist Clinic
Central Specialist Clinic
 BodyWorX Clinic
BodyWorX Clinic
 MindWorX Clinic
MindWorX Clinic
 Partner Clinics
Partner Clinics
 Family Clinic
Family Clinic
 OT&P Annerley Midwives Clinic
OT&P Annerley Midwives Clinic

