Audio newsletter version available.
Background
The Hong Kong government is currently undertaking a mass screening program for COVID-19. There are recognised challenges associated with mass testing programs[1].
We undertook an email survey in order to identify current perceptions of the testing program within our population. Our goal was to identify current barriers to testing such that we can target information to our patients and provide an evidence-based analysis to our medical colleagues in the Department of Health.
Method
The survey comprised an e-questionnaire. The questionnaire was emailed to a total of 3,044 patients. This population represented a cohort of patients who had already volunteered to be tested for COVID-19 antibodies in a previous study which we conducted in association with Hong Kong University. The questionnaire was kept live for 48 hours including the day before and the first day of the mass testing program.
Results
We received 1,013 responses giving a response rate of 33%. Responses in this survey were skewed towards older patients. Of patients who completed the survey, 72% are currently aged 35-59. Not surprisingly the demographic represents an international cohort, 84% have lived in HK for more than 6 years and 44% of patients were either born in Hong Kong or have lived here for more than 20 years.
Of patients who responded 19% indicated that they intended to register for testing and 81% indicated that they would not. There was a difference in intention to test based on both age and length of residency. Patients aged 19-34 years (9%) and those who had been in Hong Kong for 5 years or less (13%) were less likely to register than those aged 35-59 (19%) and those who had lived in HK for >20 years (22%). There will clearly be some correlation between age and length of residency. Patients born in Hong Kong were the most likely to register (24%).
The response to the question: In your opinion How well has the Hong Kong Health Department managed the COVID-19 pandemic?’ is shown below. The scale offered was from 1* for poor to 10* indicating excellent.
| How well has the Hong Kong Health Department managed the COVID-19 pandemic? | ||||||||||
| Rating | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Percentage | 1.97% | 1.58% | 3.36% | 4.84% | 8.69% | 12.34% | 26.16% | 26.46% | 9.28% | 5.33% |
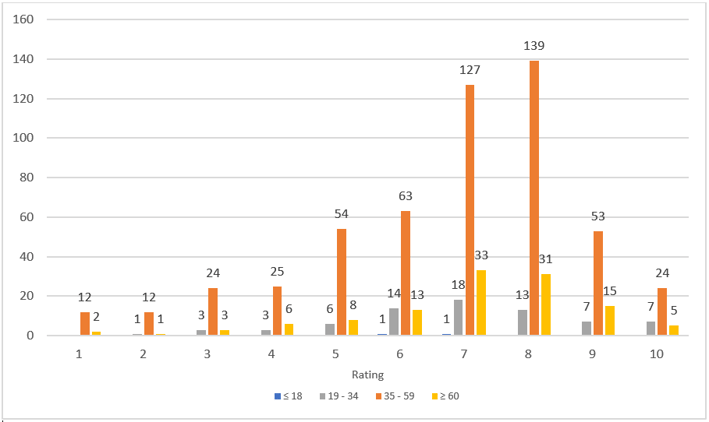
Fig. 1: An age breakdown for the question "How well has the Hong Kong Health Department managed the COVID-19 pandemic?"
The reasons given for not testing are summarised in the table below:
| Reasons | Total | Percentage |
|
I am worried about being hospitalized and/or my family members or close contacts being quarantined if the test was positive. |
291 |
35.49% |
|
I do not believe there is adequate evidence for mass testing in the current context. |
189 |
23.05% |
|
I am worried about the security and privacy of my data or DNA. |
162 |
19.76% |
|
I would prefer not to give an explanation. |
24 |
2.93% |
|
I am worried about the accuracy of the testing. |
24 |
2.93% |
|
I have already been tested. |
19 |
2.32% |
|
I am concerned about the testing environment |
13 |
1.59% |
|
Others |
98 |
11.95% |
Discussion
There are clearly limitations to this survey. The survey was an assessment of intention to test rather than a retrospective review. The OT&P demographic is not truly representative of the Hong Kong population. This cohort is more international, is skewed in terms of educational and socioeconomic factors and is generally older. The survey cohort had already volunteered for an age stratified study and younger patients are therefore under-represented in the responses. Whether this was a feature of design flaw (email versus other social media communication) or whether younger patients are less comfortable expressing an opinion would require further study. Age appears to be correlated with intention to test. At least in this population younger patients were less likely to test.
This cohort of patients have a generally favourable view of the performance of the Hong Kong Health department in the pandemic. The median rate is 7/10 and 67% of patients ranked the performance at 7/10 or higher. Notwithstanding the generally positive view of prior management, the intended uptake in the mass testing program (19%) is relatively low. How representative this cohort is of final numbers in Hong Kong will be interesting to compare.
The most important reason given for not testing is a fear of compulsory hospitalisation or quarantine of close contacts (35%). This is particularly the case for families and fear of separation from children was the most common comment in the free text responses. For patients age 19-34 years 54% see quarantine as the greatest obstruction to testing. This data is supported by comments in day to day practice. Moving towards home quarantine for close contacts and even asymptomatic positive cases has the potential to significantly increase community uptake in voluntary testing programs.
Doubts about the effectiveness of the testing program in the current context is the second most common reason given (23%). This explanation is less common in younger patients but increases with age being the most common reason given >60 years (42%). Many doctors have expressed doubts about the current program. There is a genuine academic debate about the impact of testing an entire population rather than selective samples of higher risk cohorts. There are also questions about the positive predictive value of widespread testing when the prevalence is low. This is a technical issue that means even with the best currently available testing, the likelihood of a positive result being a false positive increases as any condition becomes less common. There is general agreement amongst medical experts that more testing is good and the tests which are used are valid. The medical arguments are really over population selection, timing of testing and cost benefit.
Fears about data security or the security of DNA is the third most common concern expressed in this survey (20%).
Ultimately, education and honest information are key factors in managing epidemics of infectious disease. Politicization of health interventions from all sides of the political spectrum risks harming population health by damaging trust in public health institutions. We have consistently expressed the opinion that Hong Kong has world class systems and expertise in the management of infectious disease. There is a strong tradition of Public Health, Virology and Epidemiology which is recognised internationally. Public health interventions must balance our increasing and evolving understanding of the impact of the disease on both individuals and the health system with the social and economic costs of the interventions within the specific context of the social, cultural and economic needs of the people of Hong Kong.
Reference
1. Raffle, A., Pollock, A., & Harding-Edgar, L. (2020, August 20). Covid-19 mass testing programmes. Retrieved September 03, 2020, from https://www.bmj.com/content/370/bmj.m3262
 Central General Practice
Central General Practice
 Repulse Bay
Repulse Bay
 Clearwater Bay
Clearwater Bay
 Central Specialist Clinic
Central Specialist Clinic
 BodyWorX Clinic
BodyWorX Clinic
 MindWorX Clinic
MindWorX Clinic
 Partner Clinics
Partner Clinics
 Family Clinic
Family Clinic
 OT&P Annerley Midwives Clinic
OT&P Annerley Midwives Clinic






