All viruses have a tendency to evolve over time. The SARS-COV-2 virus has already undergone many thousands of mutations, indeed almost every single infection in Hong Kong has its own 'genetic fingerprint'. This is one of the ways we are able to connect infections to each other. We follow how closely the ‘fingerprints’ match.
What is special about the Covid mutations?
In late 2020, researchers in the UK identified a new variant. This variant is now called the Alpha variant. Different variants were also recognised in South Africa (Beta variant), Brazil (Gamma variant) and India (Delta variant). Whilst the exact position of the mutations are different they share a number of characteristics including evidence of increasing transmission rates. That is to say, these variants are more infectious. They are responsible for the sudden and rapid increase in infections which we have seen in various waves over the last year. The surge in Delta infections caused the recent increase in cases in Europe and the USA in the Autumn of 2021. Omicron is now taking over in a huge wave causing the majority of new infections worldwide.
The new variants have already spread worldwide. These variants have led to accelerations of the epidemic in the regions in which they seed. Imagine these variants as being like the iPhone. The iPhone 4 seemed like it was good at its job, but it evolved, the iPhone 5 was better and quickly became more popular. Often the evolution is gradual maybe the 5S but occasionally there is a leap, a larger screen, a better camera and over a relatively short time that particular model becomes dominant. It’s the one that everybody wants and it tends to take over. Other companies mimic the success of the most popular brand. This is the way that viruses compete. Random mutations almost always give no benefit but occasionally we find a sudden jump and the virus becomes much better at travelling, fitter and faster, they spread through the population more easily. The Delta virus was significantly more infectious than the Alpha, which itself nearly overran the US, UK and Europe in late 2020. The Delta virus spread almost everywhere in the world in 2021. Omicron is looking fitter and better at spreading than Delta. It will be the ‘most popular model’ in the world over the next few months.
What do we know about the Omicron mutation?
Viral mutations are incredibly common and the vast majority confer no benefit. We are however able to identify specific areas in the viral code which are more likely to produce a variant with an advantage. Maybe it is metaphorically the code for a bigger screen or better camera. Even then most of these mutations fail. Scientists are able to identify and track these ‘variants of concern’ to see if they get a foothold and start getting more popular. This is what has been noted with the Omicron variant which has a large number of mutations especially in the areas known to confer an advantage. It was immediately identified as ‘one to watch closely’. Having initially been found in South Africa it is now the most common variant in most countries worldwide.
Local epidemics are increasing rapidly. Data from South Africa, the UK and Denmark all show rapid growth with evidence of at least some degree of immune escape and reinfection. This suggests that the rapid growth is due to a combination of increased transmissibility and a greater ability to dodge existing immunity. All these locations have excellent testing capacity and high previous immunity from a combination of natural infections and vaccination. Data from the UK and Denmark suggests an epidemic doubling every 2 days. This suggests that a large wave of infections is on its way. It is already trending larger than the Delta wave. The early data suggests that vaccinations are less effective at preventing transmission and mild disease against Omicron than other variants. They continue to give good protection against death and severe disease. This protection is significantly improved by booster doses. More solid vaccination data will be available over the next few weeks.
The key question going forward relates to disease severity. There have been a number of reports from South Africa, the UK and Denmark suggesting that the disease associated with Omicron is milder. Whilst there are some reasons for cautious optimism, it is important to understand that South Africa is a very young population with high levels of natural immunity. The UK and Denmark also have high levels of immunity both natural and by vaccination. The impact of any variant would be expected to vary in different locations. We cannot necessarily assume that mild disease in highly immune populations would behave in the same way in infection naïve populations such as Hong Kong and China. It is also important to recognise that a large wave, of even very mild disease, can cause significant threats to a health system. A small percentage of a very large number may still be a large number over a short time. Even in South Africa the health system was under significant stress because of the numbers of healthcare workers who needed to isolate with mild infections.
Understanding the potential threat from any new variant ultimately comes down to three key questions.1. Is the new variant more infectious? 2. To what degree can the variant escape existing immunity (vaccine induced or natural)? 3. Does the new variant produce more mild or more severe disease? Data over the next few weeks will provide answers to the question about disease severity |
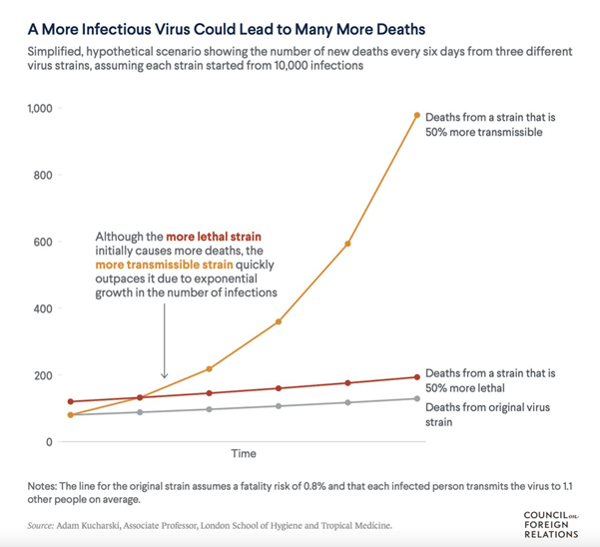
We have previously explained the important difference between the severity of disease and the severity of an epidemic. COVID-19 has the potential to overwhelm health systems because of the rapid increase in numbers. The graph below demonstrates this issue. It compares a disease which is 50% more severe, continuing with slightly higher fatality rates, versus a disease which is 50% more infectious, producing a significant increase in mortality due to the rapid increase in the number of infected cases.
It is important not to lose sight of how well the epidemic has been managed in Hong Kong. COVID-19 is a mild disease in the majority of circumstances, but it has the potential to overwhelm health systems because of a potentially rapid increase in the numbers of infected patients. Avoiding excessive strain on the hospital system is one of the main goals of the public health controls. The new variants increase the risk of an epidemic taking hold and spreading quickly. We have seen recently in New Zealand and Australia how brittle a Zero Covid strategy can be.
There are only two ways in which an individual or population can develop immunity, either by contracting the disease or through vaccination. The potential impact of these more infectious variants spreading through our densely populated city makes widespread infection a serious health threat. If an epidemic took hold in Hong Kong we would expect to see high mortality rates and significant stress to the health system. Vaccination remains the best way of developing population immunity and protecting both our population and health system. This is the reason that public health doctors are advocating so hard for population vaccination even though the current numbers in Hong Kong are so low.
In summary, we already knew that some mutations of the SARS-COV-2 virus appeared to make it more infectious. As we have previously explained, COVID-19 is not a serious disease in the majority of circumstances but rather it is the nature of the epidemic and particularly the tendency to overwhelm health systems which causes harm. The real challenge now is to overcome vaccine hesitancy and drive vaccination rates higher, especially in the older and most vulnerable proportion of the population.
We will continue to share evolving evidence on our website and here. For anyone who wishes to follow evolving Omicron data, we will share reputable sources of data here![]()
 Central General Practice
Central General Practice
 Repulse Bay
Repulse Bay
 Clearwater Bay
Clearwater Bay
 Central Specialist Clinic
Central Specialist Clinic
 BodyWorX Clinic
BodyWorX Clinic
 MindWorX Clinic
MindWorX Clinic
 Partner Clinics
Partner Clinics
 Family Clinic
Family Clinic
 OT&P Annerley Midwives Clinic
OT&P Annerley Midwives Clinic

